Learn how to use HCC RAF Score tools and Get started.
Use Case #5 for our HCC RAF Score Tools
How to easily gain providers’ support to act on provider education reports in concurrent coding for Risk Adjustment?
Problem:
The concurrent review primarily involves fee for service coding, which also includes Risk Adjustment
coding in most healthcare organizations. In Fee for Service coding, all
eligible ICDs are associated with E & M Codes and are processed. Conversely, Risk Adjustment coding
focuses solely on ICDs linked to the Hierarchical Condition Category
(HCC) following the MEAT rules. Risk Adjustment coders review patient charts and document diagnosis (Dx)
codes requiring addition, deletion, modification, or marking as
unchanged, along with the necessary medical evidence for HCC conditions.
Medical coders generate provider education reports using cumulative monthly diagnostic data, both at the
patient and provider levels, which are then shared with healthcare
providers. These reports typically provide information about changes, additions, deletions, and
modifications of diagnosis codes. However, in many instances, these changes
may involve diagnosis codes with the same Hierarchical Condition Category (HCC) value. Consequently,
providers may not give significant attention to these findings
Our Solution:
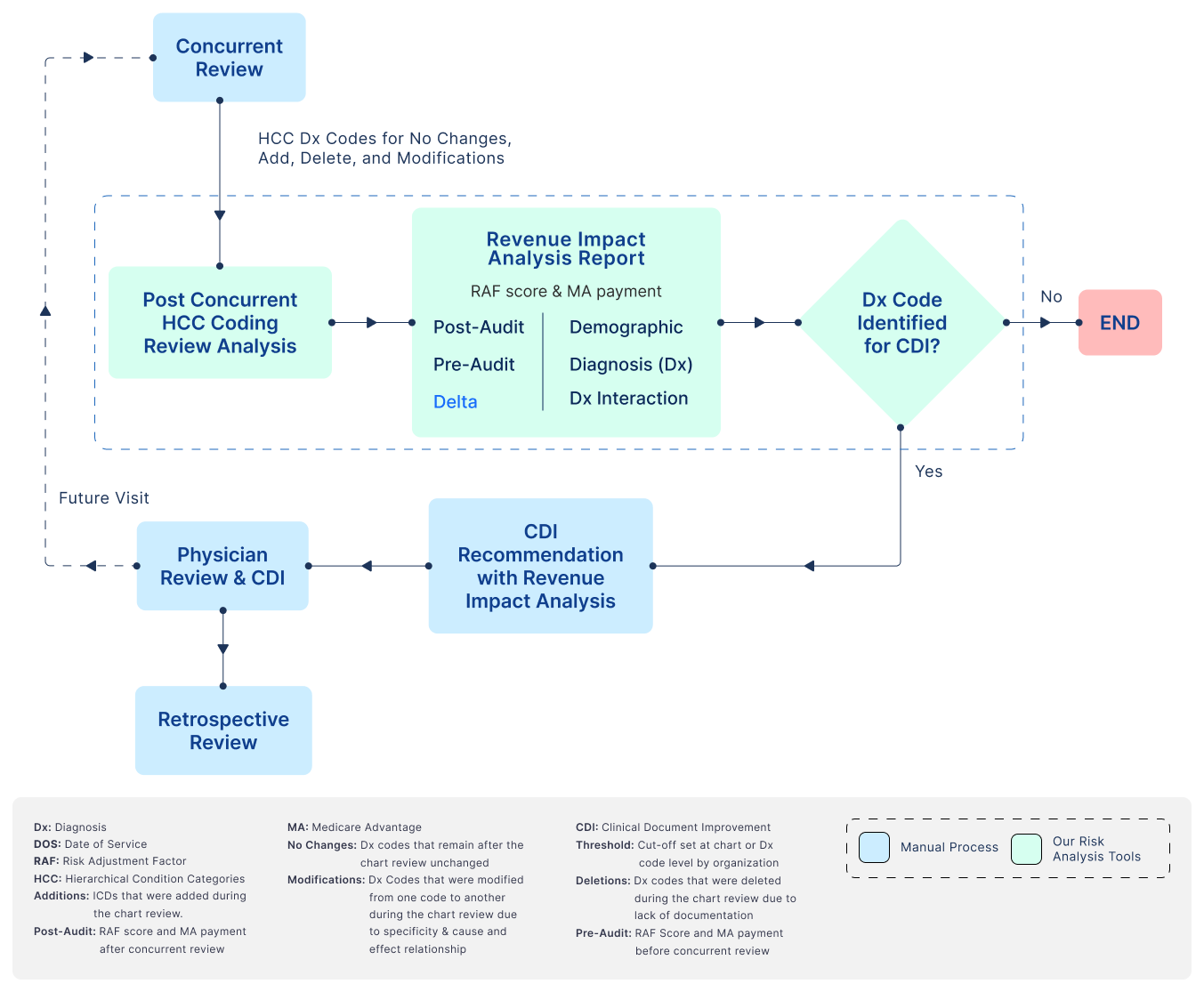
To address this issue and ensure that providers act on relevant diagnosis code changes, we have designed RAF Score Tools, these tools analyze diagnosis codes and demographic data and provide accurate recommendations regarding high-priority and low-priority codes based on RAF scores and their associated revenue impact in Medicare advantage payment. When medical coders share the provider education report, including RAF scores and revenue impact for high-value diagnosis codes, providers are more likely to engage with the report and act upon it.
Benefits:
-
Increased Provider Engagement:
By presenting physicians with a clear distinction between high and low-revenue impact diagnosis codes, they are more likely to pay attention to the education report and take appropriate actions to improve documentation and coding accuracyò
-
Enhanced Revenue Capture:
Our approach ensures that physicians receive only diagnosis codes with a significant revenue impact for Clinical Documentation Improvement (CDI) efforts. This targeted approach directly contributes to enhanced revenue capture, as it focuses on the areas with the greatest financial potentialò
-
Efficient Resource Utilization:
Healthcare organizations can allocate CDI resources more efficiently. Instead of dedicating equal effort to all diagnosis codes, CDI specialists can prioritize their work on high-revenue impact diagnosis codes, saving time and resources
Our Tools:
Watch the step-by-step HCC Medicare RAF Score Tools Video Demos.
Learn about 5 important use cases where HCC RAF Score tools can be used.

